
September 13, 2024
Management Of Urinary System Incontinence In Postmenopausal Females: An Emas Clinical Overview
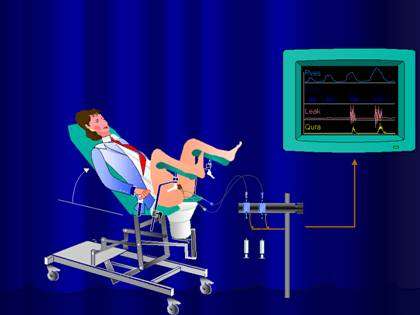
Administration Of Urinary System Incontinence In Postmenopausal Ladies: An Emas Scientific Guide They'll first intend to try things that have the least effect on your body. Info provided on the Aeroflow Urology blog Nocturia is not planned as a substitute for clinical advice or care from a health care specialist. Aeroflow recommends consulting your healthcare provider if you are experiencing clinical problems associating with incontinence. Additionally called Kegel workouts, these exercises can aid improve the stamina of your pelvic flooring. Even if you don't have urinary incontinence, you must do pelvic floor workouts to aid maintain your pelvic area strong and continent. The variation of progesterone and estrogen is why you experience signs and symptoms throughout your cycle and while on your duration. Later on, in a subgroup of these people, myopathic adjustments may happen in the bladder that make the spread of extraordinarily created contractile signals more efficient and harder to reduce voluntarily. These connective-tissue elements form the passive supports to the urethra and bladder neck. During times of increased intra-abdominal stress, if these assistances are undamaged, they enhance the encouraging result of muscular closure of the pelvic flooring. INNOVO's distinct Multipath ™ Modern technology makes sure optimal muscle engagement and effectiveness, delivering targeted stimulation to the pelvic flooring muscular tissues without the requirement for intrusive probes or hand-operated intervention.Therapies
These hormone changes can influence bladder feature and urinary system behaviors, showing up as urinary system signs such as enhanced frequency, seriousness, or leakage. Low degrees of estrogen and urinary system incontinence go hand in hand. As ladies age and begin coming close to menopause, the ovaries slow down the procedure of making estrogen, and the levels of this female sex hormonal agent naturally decline in the body. [newline] Eventually, with menopause, the production of estrogen quits, and this affects the body in lots of methods. Without estrogen, women find it challenging to maintain healthy urologic features throughout and after menopause. Bladder control for women starts along with their final menstrual duration and increases thereafter.How Is Incontinence Treated?
Urethral inexperience normally causes intermittent urinary incontinence, typically at rest. Hormonal agent therapy (estrogen) in postmenopausal females alleviates urinary regularity which leads to enhance in the stamina of muscle mass around the bladder. Althoughbasic science in this field is limited, a recent placebo-controlled, randomizedclinical trial of estrogen alone clarifies this concern. Urethral closureis based on the incorporated action of the suburethral vaginal wall, thepubourethral tendons, the pubococcygeus muscles, and the paraurethral connectivetissues. As you age, the muscle mass that sustain your pelvic organs can weaken. This means that your bladder and urethra have much less support-- frequently bring about pee leak. At rest, the urethra has a greater intrinsic stress than the bladder. This pressure slope relationship is protected if severe rises in intra-abdominal stress are transferred equally to both body organs. The 2nd mechanism entails intact connective cells support to the bladder neck and urethra.- Case or worsening of symptoms focused on tension, impulse, and mixedUI reported at baseline and 1 year.
- People with urinary incontinence commonly deal with this condition for 6-9 years before seeking clinical treatment.
- The hollow member by supporting muscles is put in a best location and if for any kind of factor the sustaining muscular tissues shed the ability, bladder displaced from its location and creates problems for the individual.
- Cauda equina disorder can establish in patients with a big centrally extending disk.
Is urinary bladder under hormonal control?

Social Links