September 1, 2024
Pee Urinary Incontinence An Introduction
Problems
What hormone quits pee?
earn less pee during the night. Takeaway: If progesterone degrees are rising during and after your cycle, and progesterone creates your bladder to get extra regularly, it may create incontinence. Menstrual changes. There are several reasons your regular monthly period can transform, but hormonal discrepancy typically plays a role.Hair problems.
Alternative Treatments And Management
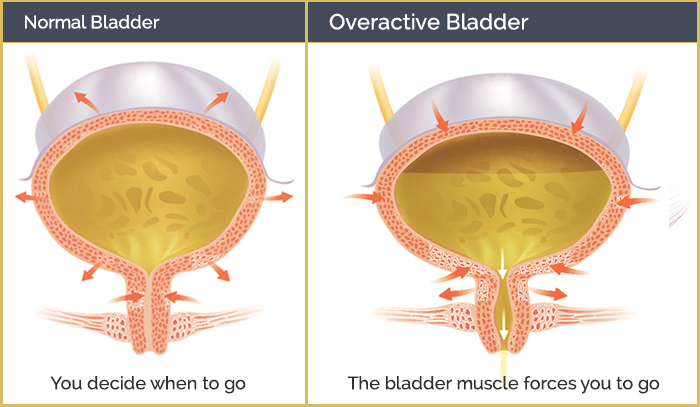
Figure out if you certify to get urinary incontinence supplies totally free through your insurance at the bottom of the page. An individual needs to consult with a doctor if they have any kind of issues they may have low estrogen or if they are experiencing bladder signs. Low estrogen can likewise affect people outside of menopause, specifically after delivering or during breastfeeding. As lots of as 15% of premenopausal females might have GSM-like signs because of this. Nonetheless, they can likewise go down throughout other phases of life, such as after giving birth or while breastfeeding. Later, in a subgroup of these people, myopathic modifications might take place in the bladder that make the spread of abnormally generated contractile signals more effective and more difficult to reduce willingly. These connective-tissue parts develop the passive supports to the urethra and bladder neck. Throughout times of enhanced intra-abdominal pressure, if these supports are intact, they enhance the helpful effect of muscular closure of the pelvic floor. INNOVO's unique Multipath ™ Modern technology ensures optimal muscle mass interaction and effectiveness, providing targeted excitement to the pelvic floor muscle mass without the demand for invasive probes or hand-operated intervention. In Website link addition, the patient relearns just how to control the bladder and enhance the included muscular tissues. Urinary bladder hypocontractility or poor holiday accommodation of urine throughout storage may cause regular leak of little volumes of urine. Disorder may be caused by urinary system system infection, chronic inflammatory conditions, neoplastic lesions, exterior compression, and chronic partial outlet obstruction. It also helps maintain your bladder and urethra healthy and balanced and working appropriately. They might no more be able to control your bladder as they did before. As your estrogen levels remain to drop throughout and after menopause, your UI symptoms might become worse. Estrogens, usually in the form of diethylstilbestrol, are administered to spayed women.- Subtle obstruction and the impacts of aging on smooth muscle and the autonomic nervous system are 2 possible contributors.
- If you have a persistent problem like diabetes or multiple sclerosis, you may have urinary incontinence for a. extended period of time.
- The suggested dosage is 1.5 to 2.0 mg/kg twice daily to three times daily.
- Often it is the very first and just signs and symptom of an urinary tract infection.
Social Links