September 1, 2024
Physiotherapy In Females With Urinary Incontinence
Medical Management Of Male Anxiety Incontinence Rru In summary, SUI can be shown in women with POP without signs of SUI after POP reduction in approximately 30% of instances. Treatment of nocturia in OAB individuals with anticholinergic medications reveals reduction in nocturia episodes. Desmopressin treatment for nocturia shows significant reductions in nocturnal pee output, nocturnal urinary regularity, and nighttime polyuria index. Deal urethrolysis to ladies that have nullifying difficulties after anti-UI surgical treatment. Deal urethral dilatation to females with urethral constriction causing BOO but suggest on the most likely requirement for duplicated treatment.- A SR of non-randomised studies found no differences in UTI end result or UUT adjustments in between use suprapubic or urethral catheter drainage; nevertheless, individuals with suprapubic catheters were less likely to have urethral issues [121]
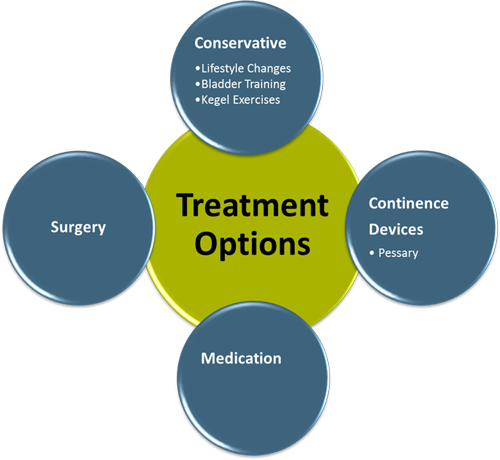
- Anticholinergics, like Oxybutynin (Ditropan), can be used to relax over active bladder muscle mass.
- Clashing evidence originates from a SR assessing the efficiency and issues of different procedures for women recurrent SUI and reported on data from 350 females in 10 RCTs with a mean follow-up of 18.1 months [416]
Useful Mind Imaging And The Neural Basis For Voiding Disorder In Older Grownups
Valsalva leak factor stress did not dependably evaluate urinary incontinence intensity in a friend of women selected for surgical treatment of SUI [69] Procedure post-void recurring (PVR) quantity, especially when analyzing patients with nullifying signs or complicated tension urinary incontinence (SUI). Urinary diversion stays a rebuilding choice for individuals with intractable UI after several pelvic procedures, radiotherapy or pelvic pathology resulting in irreparable sphincteric inexperience or fistula development. Options include ileal conduit urinary system diversion, orthotopic neobladder and heterotopic neobladder with Mitrofanoff continent catheterisable channel. There wants evidence to talk about which procedure leads to the most better QoL.Suburethral Sling Procedure
It was concluded that short-term end result of PFMT can be preserved at lasting follow-up without incentives for continued training, however there is a high diversification in both interventional and technical high quality in short- and lasting PFMT research studies [328] A Cochrane evaluation contrasted PFMT without treatment or inactive control treatment and found that ladies with SUI in the PFMT teams were 8 times more probable to report treatment [316] The testimonial also documented considerable renovation in SUI and improvement in UI QoL. Pelvic floor muscle mass training decreased leak by an average of one episode per day in females with SUI.What is the best treatment for urinary incontinence?

Social Links