September 7, 2024
Urinary System Incontinence: Therapy, Creates, Kinds, And Symptoms
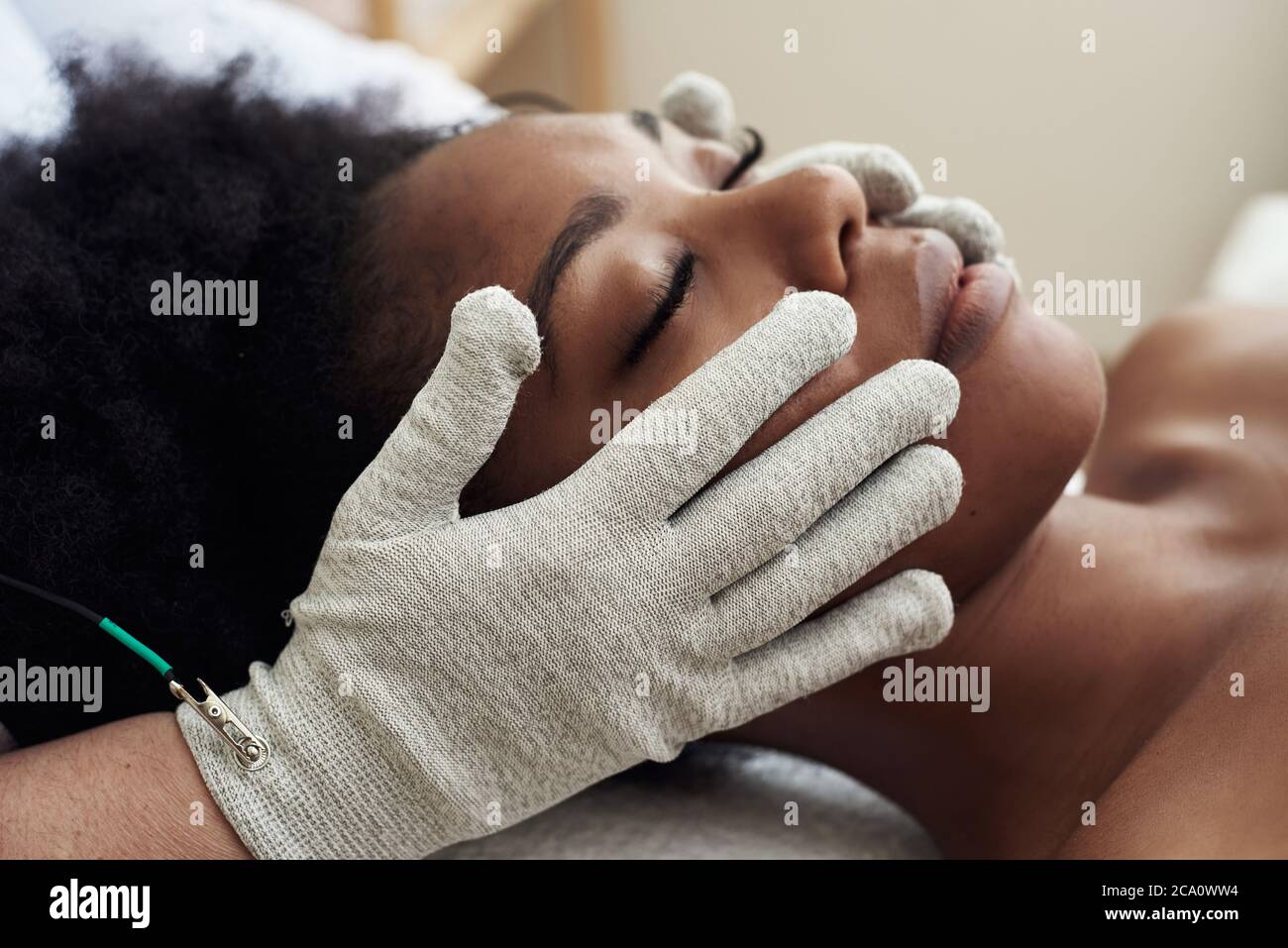
Urinary System Incontinence Symptoms And Causes Therapy options array from Botox shots to targeted workouts, biofeedback and electric excitement to reinforce the pelvic floor muscles. Diagnosis of MUI typically includes an in-depth clinical Rejuvenate history and straightforward workplace tests, including urinalysis, postvoid recurring urine quantity dimension, and pelvic evaluations. Treatment alternatives range from conservative methods (eg, way of living adjustments and pelvic floor exercises) to more intrusive treatments for instances unresponsive to preliminary treatments.What is the 2nd line treatment for urinary system incontinence?
What Is The Most Effective Medication For Bladder Control?
Later, detrusor hyperreflexia typically is located upon urodynamic evaluation. Since the bladder neck and proximal urethra vacate the pelvis, even more pressure is transferred to the bladder. During this procedure, the posterior wall surface of the urethra shears off the anterior urethral wall to open up the bladder neck when innate sphincter shortage exists. Urinary urinary incontinence in women is not a current clinical and social sensation, yet the relative significance attributed to urinary incontinence as a medical problem is increasing. Numerous elements in charge of the increased interest to urinary incontinence can be mentioned.Remain On Top Of Most Current Health And Wellness News From Harvard Medical School
These ring- or dish-shaped devices normally are strengthened in the location that rests under the bladder neck/proximal urethra. A degree of success has been accomplished with these specially made pessaries. Urethral occlusive devices are artificial devices that may be put right into the urethra or placed over the urethral meatus to avoid urinary system leakage. These tools are palliative measures to stop involuntary pee loss.- The workouts contain volunteer tightenings of the muscular tissues of the pelvic flooring.
- The death rate of retirement home citizens with urethral catheters has been discovered to be 3 times more than for citizens without catheters.
- A small research study revealed a 90% improvement price in 20 patients with detrusor instability that was unresponsive to pharmacotherapy.
- If you have overflow urinary incontinence or you can not fully vacant your bladder, you may need to make use of a catheter.
- Bladder control issues occasionally continue even after making lifestyle adjustments and trying bladder training.
- Urinary urinary incontinence can lead to prolonged healthcare facility admission, urinary system tract infections, call dermatitis, and falls.
Social Links