:max_bytes(150000):strip_icc()/GettyImages-1156991077-63abeae534eb4abb88a83863c8c11928.jpg)
September 10, 2024
Impact Of Conjugated Estrogen In Stress Urinary System Incontinence In Ladies With Menopause
Understanding The Web Link Between Reduced Estrogen Levels And Urinary System Incontinence
The treatment resulting in lower testosterone levels can deteriorate the pelvic flooring muscle mass, leading to UI. As a result, treatments such as pelvic exercises may be essential in taking care of UI if you are getting ADT. Additionally quit the circulation of urine in midstream urine creates to strengthen the pelvic floor muscle mass.Reasons To Select Laparoscopy Over Conventional Treatment
These cyclical variations in urinary habits highlight the elaborate interaction between hormonal fluctuations and bladder function throughout the menstruation. Talk with your healthcare provider regarding these home therapy options for incontinence before beginning any one of them. You may not have Nocturia the ability to treat all sorts of incontinence with these way of living adjustments. Your carrier could also make comprehensive tips to you about the most effective lifestyle adjustments to try offered your incontinence medical diagnosis. It causes you to leak urine because your bladder is too complete or you can not completely empty it. The bladder is a sac like body organ that is inside the pelvis and its duty is to hold pee that from kidneys and through ureter pipe is dripping right into it. The hollow member by sustaining muscular tissues is put in a right place and if for any type of reason the sustaining muscle mass lose the capacity, bladder displaced from its area and produces issues for the person.- Endocervix glandular cells activity throughout menopause and subsequently the quantity of mucin reduces that this triggers to vaginal dry skin that occurs as a primary grievance in postmenopausal females.
- Urge urinary incontinence is more prevalent after the menopause, and the optimal frequency of tension incontinence happens around the moment of the menopause.
- These hormone shifts can affect bladder feature and urinary system behaviors, manifesting as urinary signs and symptoms such as increased regularity, seriousness, or leak.
- Stress urinary incontinence establishes when activity puts raised stress on your bladder.
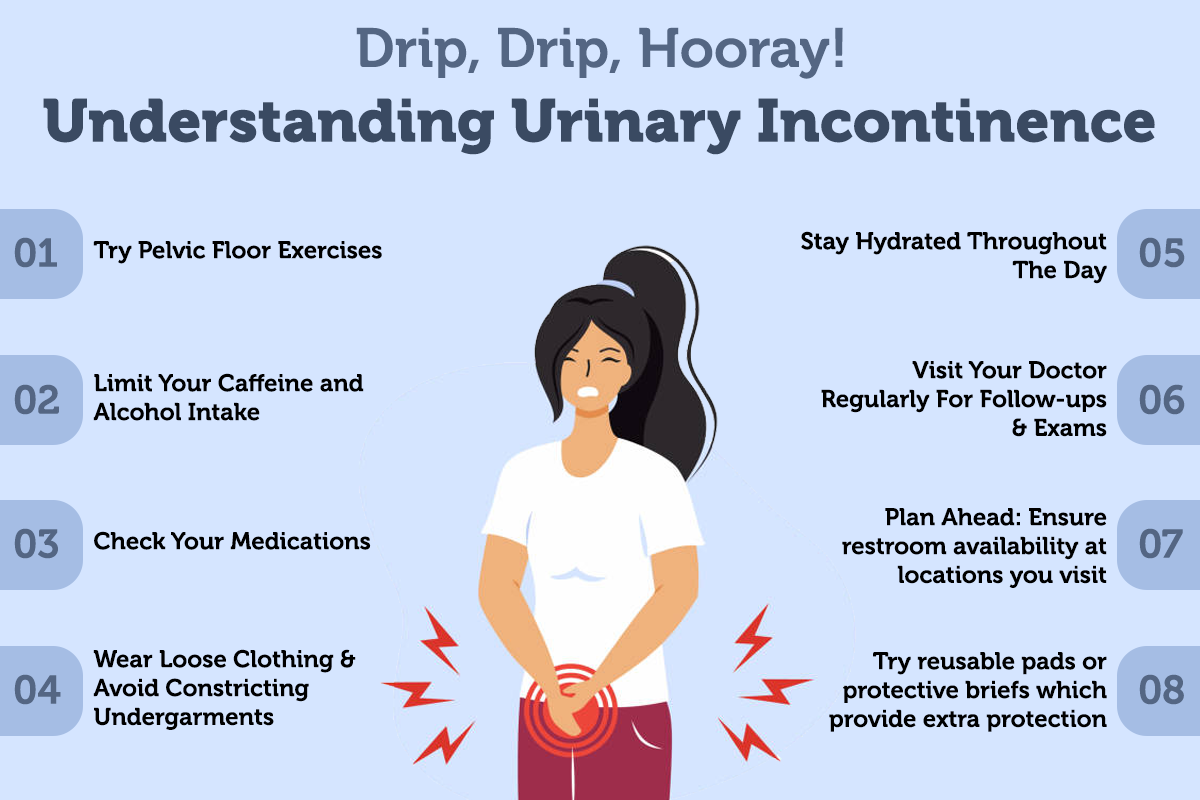
Just how can bladder leak be quit?
and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and rest issues.Digestive distress. Applying low-dose, topical estrogen may aid. The drug is available in the form of a genital cream, ring or spot. The estrogen may aid bring back the cells in the vaginal area and urinary system system to ease some symptoms. Topical estrogen may not be risk-free for people with a history of bust cancer, uterine cancer cells or both. Summary. Bladder dysfunction is an usual challenge, particularly later on in life and during times of major hormone modification. Reduced estrogen bladder signs and symptoms can include incontinence, overactive bladder, and pain.

Social Links