
September 1, 2024
Monitoring Of Urinary Incontinence In Postmenopausal Ladies: An Emas Clinical Guide
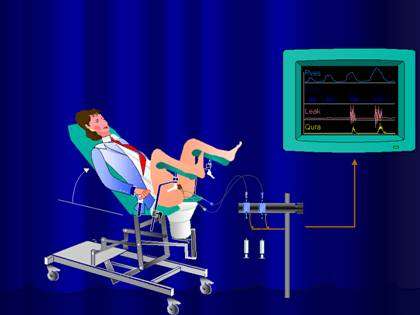
6 Methods To Treat Bladder Leakage Hormone Substitute Treatment (HRT) is a type of therapy that entails the management of hormones, especially estrogen, progestin (a type of progesterone), or both. A lady's body quits generating these hormones after menopause, causing conditions such as urinary system incontinence. Reestablishing the hormonal agents in numerous forms, including pills, spots, creams, and genital rings, can aid turn around the impacts of these conditions. Urinary system urinary incontinence (UI) is also known as "loss of bladder control" or "spontaneous urinary system leak." Numerous women experience it, and the frequency of UI tends to increase as you get older. 1) Urodynamic examination where stress of bladder and urethra are gauged. It does not seem that the initial reason of dystrophy or carcinoma of exterior genitalia is estrogen deprival. Hit to genital may be accountable for about 15 percent of bleeding after menopause, and on the various other hand, the incidence of Vaginitis throughout the years after menopause boosts. Some believe that certain children develop a pattern of not loosening up the pelvic flooring while voiding. Sometimes, this can be mapped back to an infection or some other poisonous stimuli. A vicious cycle of pelvic floor convulsion, constipation, and urinary system retention can develop.
Checklist Of Reduced Estrogen Bladder Signs
These hormonal changes can influence bladder function and urinary system practices, manifesting as urinary system signs and symptoms such as enhanced regularity, seriousness, or leakage. Reduced degrees of estrogen and urinary system incontinence go together. As ladies age and start approaching menopause, the ovaries decrease the procedure of making estrogen, and the degrees of this women sex hormone normally decrease in the body. [newline] Ultimately, with menopause, the production of estrogen quits, and this impacts the body in numerous methods. Without estrogen, females locate it hard to maintain healthy urologic functions during and after menopause. Bladder control for ladies starts alongside their final menstruation period and enhances after that.Information From Mayo Center
Urethral inexperience generally results in periodic urinary incontinence, generally at rest. Hormone treatment (estrogen) in postmenopausal females minimizes urinary frequency which brings about raise in the stamina of muscle mass around the bladder. Althoughbasic scientific research in this field is limited, a recent placebo-controlled, randomizedclinical test of estrogen alone sheds light on this problem. Urethral closureis depending on the incorporated action of the Go to this site suburethral genital wall, thepubourethral ligaments, the pubococcygeus muscular tissues, and the paraurethral connectivetissues. As you age, the muscular tissues that sustain your pelvic organs can compromise. This implies that your bladder and urethra have less assistance-- frequently resulting in pee leakage. Discover if you certify to receive incontinence materials free through your insurance at the end of the web page. A person needs to speak to a doctor if they have any worries they might have low estrogen or if they are experiencing bladder symptoms. Low estrogen can additionally affect people beyond menopause, especially after giving birth or during breastfeeding. As many as 15% of premenopausal women may have GSM-like signs consequently. However, they can also drop during other stages of life, such as after delivering or while breastfeeding.- People with incontinence typically live with this problem for 6-9 years before looking for medical treatment.
- Biofeedback is coordinated with pelvic flooring (Kegel) exercises.
- The hollow member by sustaining muscle mass is positioned in a right location and if for any kind of factor the sustaining muscular tissues shed the capacity, bladder displaced from its place and produces problems for the individual.
- Consequently, the prevalence of urinary system incontinence reported in the literature is varied.
- Cauda equina syndrome can develop in individuals with a big centrally protruding disk.
Exactly how can bladder leak be quit?
and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and rest issues.Digestive distress. Applying low-dose, topical estrogen may aid. The medicine can be found in the kind of a genital lotion, ring or patch. The estrogen might help recover the tissues in the vaginal area and urinary system system to ease some symptoms. Topical estrogen could not be risk-free for people with a history of breast cancer cells, uterine cancer cells or both. Summary. Bladder dysfunction is a typical difficulty, particularly later on in life and throughout times of major hormone adjustment. Low estrogen bladder signs and symptoms can consist of urinary incontinence, over active bladder, and discomfort.
Social Links
